A frequently asked question is: “What happens to your body when you have gout?”
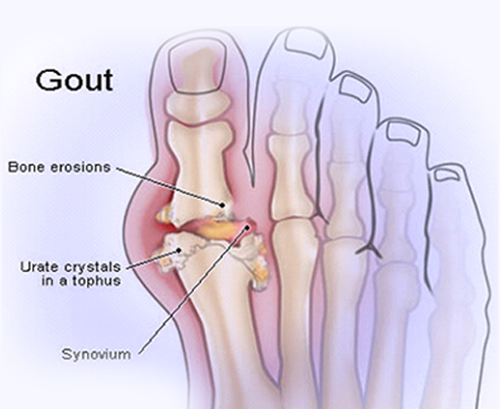
Gout is a type of arthritis. It is caused by the buildup of uric acid crystals in the joints, also called hyperuricemia.1 Gout often occurs in the big toe and may show up in other body parts, such as the heels, instep, ankles, knees, elbows, hips, thumbs and fingers. Acute gout usually appears suddenly, in the form of an extremely painful joint that is red, hot and swollen.2
The progress of gout has four stages:2-4
Hyperuricemia. This stage of gout has no symptoms. Uric acid levels are elevated, but no symptoms have yet occurred.
Acute gout. Hyperuricemia has caused uric acid crystals to form deposits in joint spaces, often in the big toe. An acute attack often begins at night, with intense pain. It can be triggered by stress, use of alcohol or certain medicines or an illness. Most attacks, also called flares, will subside within three to 10 days, and another may not occur for months or years. Without treatment, however, subsequent attacks last longer and occur more often.
Interval/intercritical gout. The period between attacks when no symptoms are present.4 After the initial attack, 62% of participants in a study of 208 people with gout had another attack within a year. In that same study, 78% of patients had another attack within two years. After 10 years, 93% of the patients reported at least one more attack.5
Chronic tophaceous gout. This stage of gout can take as many as 10 years to develop. It can be disabling, causing permanent damage to joints. It can damage the kidneys as well.4
In people with advanced gout, the urate crystal deposits can get large enough to form white or yellow lumps under the skin. These lumps are called tophi (pronounced TOE-fye). Tophi can develop on the hands, fingers, feet and toes, as well as in the Achilles tendon along the back of the ankle. They can become swollen and extremely painful during gout flares. Tophi on the hands can be especially problematic because they can make it difficult to prepare food, fasten buttons and perform other tasks of daily life. Proper treatment by a doctor may prevent gout from reaching this stage.6,7
When uric acid builds up in the kidneys, it can cause large stones. These stones, which are painful, can cause permanent damage by obstructing kidney function, causing infection, and scarring the tissues with their rough or sharp edges. To help prevent this kind of damage, see your doctor for a proper diagnosis and treatment. Prescription medication is available to help prevent gout flares in adults. It is also important to make the lifestyle changes your doctor recommends.6
Many gout symptoms, such as swollen joints and tophi, are obvious. However, gout may be linked to other health problems that are harder to recognize. Research has shown that excess uric acid in the body has been associated with a high risk of death from heart conditions. In addition, studies have found that there is a link between gout and metabolic syndrome. Metabolic syndrome is the name for a group of risk factors such as excess abdominal fat, high blood pressure, high triglycerides and low “good” cholesterol. Having metabolic syndrome can raise your risk of heart disease and diabetes.8
People with gout can affect the course of the disease by following certain lifestyle guidelines. These include avoiding foods that are high in purines (such as liver, organ meats, shellfish, oily fish and high-fructose corn syrup), eliminating alcohol, limiting sugar intake, exercising (and losing weight, if necessary) and staying well hydrated.7
For answers to other common questions, see our FAQs for Patients.
NOTE: This article was not written by a medical professional and is not intended to substitute the guidance of a physician. These are not West-Ward’s recommendations for gout flare prevention, but rather facts and data collected from various reliable medical sources. For a full list of resources and their attributing links, see below.
